What Are Bone Marrow Lesions (BMLs)?
Fast Facts On Bone Marrow Lesions:
-
- Cause: Osteoarthritis; stress fractures; bone infections
- Primary Symptoms: Joint pain
- Prognosis: With targeted therapies, bone marrow lesions are treatable and reversible
What Are Bone Marrow Lesions (BMLs)?
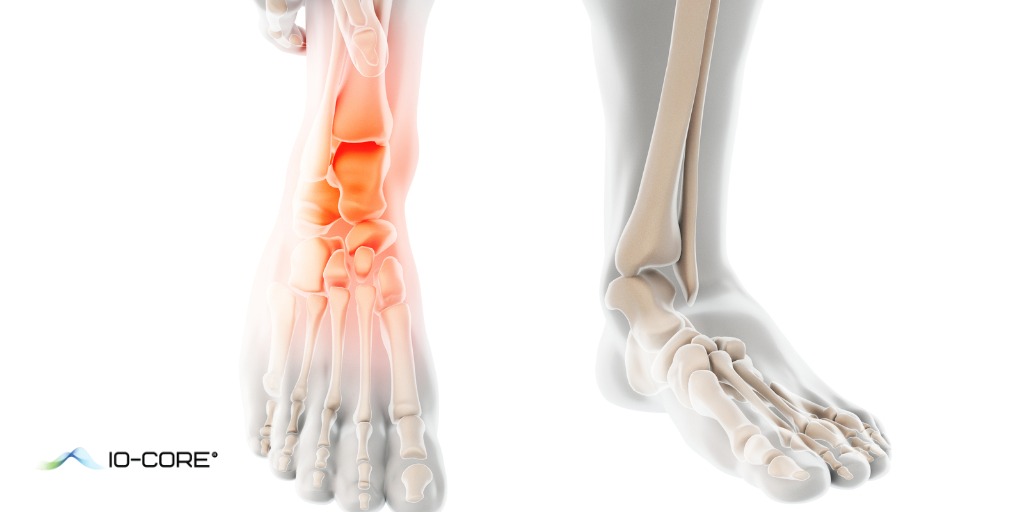
The terms bone marrow edema and bone marrow lesions (BML) can be used interchangeably. When BMLs were first seen on MRI studies, scientists believed they were areas of fluid build-up in bone marrow. With further research, scientists have discovered that BMLs are composed of multiple factors, and thus the term “bone marrow lesion” was introduced.
Bone marrow lesions are a study in progress, and there is a lot of information scientists don’t know about what causes these lesions, what they’re made of, and how they affect the human body and disease process. Right now, what we do know is that BMLs present frequently in the setting of osteoarthritis (OA) and the presence of lesions may be an early indicator of OA in patients.
Concerning the composition of lesions, we know that BMLs are areas of high metabolic activity within the bone marrow space. They may contain normal tissue, fibrosis, necrosis, bleeding, edema and microfractures.
Bone marrow lesions can develop in the setting of any medical condition or injury that affects the structural integrity of bone and they can develop on any bone in the body. Depending on the cause, the lesions are treatable and reversible.
How BMLs Affect the Progression of Arthritis
Much of researchers’ knowledge of bone marrow lesions has come from studying them in the setting of osteoarthritis. For many years, the prevailing belief was that damage from OA only affected the articular cartilage that covers joints. Today, new research suggests that OA affects not only the surface cartilage, but the underlying bone (called the subchondral bone), ligaments, synovial membrane and other structures that make up the joint.
Bone marrow lesions are believed to be a result of structural damage to the subchondral bone caused by osteoarthritis. In OA patients, BMLs have been linked to increased pain, rapid progression of the disease and increased risk of cartilage loss.
Traditional treatments for osteoarthritis focus on reducing symptoms, preserving joint mobility and slowing the progression of cartilage loss. However, new research suggests that therapies targeting bone marrow lesions and restoration of bone integrity can provide significant pain relief and slow down the progression of OA.
Causes
Bone marrow lesions have been discovered in the setting of multiple conditions, including:
- Degenerative arthritis
- Osteoarthritis (OA)
- Inflammatory arthritis
- Rheumatoid arthritis (RA)
- Ankylosing spondylitis
- Psoriatic arthritis
- Metabolic arthritis
- Gout
- Bone and joint infections
- Osteomyelitis
- Septic arthritis
- Cancer/tumors
- Trauma
- Stress fractures
- Compression fractures
- Insufficiency fractures
- Bone bruises
- ACL tears
Diagnosis
Bone marrow lesions can’t be visualized on an X-ray or CT scan. An MRI or ultrasound is necessary to detect BMLs. They present as areas in the bone with high water signals.
Treatment Options
Because there is still so much scientists don’t know about bone marrow lesions, there is no medical consensus on the best treatment options. Several of the treatments listed below have shown promising results in existing studies, but more research is necessary to determine the effectiveness of treatments.
Conservative Treatments
Conservative treatments aim to reduce symptoms and maintain or improve joint function, but don’t address BMLs directly. Studies comparing BMLs before and after conservative treatments revealed no change in the lesions’ size and appearance in patients with osteoarthritis.
Conservative measures include pain medications, rest and offloading, physical therapy and cortisone injections. While the above treatment methods can help reduce pain, inflammation and stiffness, they can’t restore the integrity of the underlying bone, prevent the progression of damage or slow the disease process.
Surgery
In patients with OA, total joint replacement is performed when patients can’t find relief from conservative treatment options. Unfortunately, joint replacement surgery may include risks: replacement surgeries are invasive, expensive and require months of rehabilitation afterward to regain functionality in the joint. According to the journal of Bone and Joint, “approximately 22% of patients experience chronic pain” after total knee arthroplasty.
Core Decompression
Core decompression is a surgical procedure that involves drilling tiny holes in the damaged bone surrounding the joint. The goal is to relieve pressure and improve blood flow in the area to promote healing.
Advancements in core decompression procedures include combining core decompression with a small, healthy bone graft and an injection of stem cells. This treatment method introduces growth factors into the damaged area and promotes bone regrowth and healing. The possible downside is that core decompression may only slow or delay further bone and joint damage, instead of treating it completely.
Medications
Two types of medications may help relieve pain in patients with BMLs. Prostacyclin is a vasodilator that promotes bone regeneration. Bisphosphonates are used to treat multiple bone diseases because they help prevent the breakdown of bone. Existing studies show that both medications can reduce pain, improve functionality and reduce the appearance of lesions. The possible downside is that medications only reduce or mask symptoms, but don’t treat bone and joint damage.
Prevention and Lifestyle Changes
Bone marrow lesions aren’t always preventable, especially if they’re caused by a degenerative condition like osteoarthritis. However, there are steps you can take at home to protect your joints and reduce your risk of injury.
- Exercise. Regular exercise improves joint flexibility and mobility, and builds strength in the surrounding muscles. Mix up your exercise routines to include a balance of low-impact and high-impact activities. High-impact activities like running can cause repeated microtrauma to your joints. Walking, water exercises, swimming and bicycling are low-impact exercises that improve strength while taking pressure off the joints.
- Lose weight. Maintain a healthy weight for your body type. Being overweight places more stress on your weight-bearing joints.
- Support your joints. Practice using proper posture when you stand, sit and walk to distribute your weight equally across your joints. Wear properly fitting shoes that have arch and heel support to reduce pressure on your knees, hips and back when you walk.
If you’ve been diagnosed with arthritis or joint damage and you suffer from pain, stiffness and difficulty walking, climbing stairs or performing daily activities, then the iO-Core™ procedure may be a viable treatment option for you. iO-Core™ combines orthopedics and biologics to treat degenerating cartilage and underlying bone and tissue damage caused by arthritis and other joint injuries. Treating the underlying damage and not just the surface layer of cartilage has shown better results in decreasing pain and improving mobility for many patients. Contact us today to see if you qualify for the iO-Core™ procedure.